No matter how old your child gets, they’re still your kid, and you’re still going to be worried about them. Are they happy with their career? Are they managing their money well? Do they have friends they still hang out with? Are they being safe when they’re out and about?
When you swing by to visit them, you do your best not to snoop, but you observe their living situation. Are they keeping it clean? Do they have enough food in their fridge? You just want what’s best for them and you’re worried they won’t ask for help if they need it.
Sometimes our fears are unnecessary, but other times they get confirmed. This happens for nearly 1 in 8 families here in Arizona. 13.7% of young adults aged 18-25 in Arizona reported having a substance use disorder within the past year. As a parent, seeing your child dealing with substance use during any period of their life, can make you feel helpless. You can’t send them to their room like you used to, so what can you do? Is it somehow your fault? Is there something you could’ve done if you had noticed sooner?
You’re not alone in feeling this way. Drug use affects many families in the Phoenix area, and the state of Arizona as a whole. From 2020 to 2022 overdose deaths in Maricopa County have increased by 30%. Nearly 17% of people age 18+ in Arizona report binge drinking at least once a month. Sometimes we read these statistics and all we see are numbers on a page or screen, but every number represents a family like yours, hurting because of their loved one’s substance use or alcohol use disorder.
Our team at Pinnacle Peak has seen over the years exactly how much substance use and alcohol use can impact not only families but our communities as a whole. We know how overwhelming it can feel when you don’t know what you’re dealing with, nor what steps are right to take to help someone.
In this guide, we want to help bring clarity and answers to some of the most common questions you may have about substance use and recovery. 75% of people who have had a substance use disorder in their lives find recovery. It’s never too late to start and there’s always hope for tomorrow.
During your read, we encourage you to check the table of contents to find answers to questions you may have. This guide will be broken down into chapters focusing on specific topics to make it easier for you to find the information you need. If at any time you have additional questions or wish to know more about our treatment options, you can give us a call at 866-377-4761. There are resources designed to support you and your loved one in a recovery journey.
At Pinnacle Peak Recovery our goal is not to scare you into making a rash decision about your adult child’s care but to give you useful information so that you know you are making sound decisions, and to give you the hope that recovery is not only possible, it is likely!
Chapter 1: The Basic of Substance Use Disorders
What Is a Substance Use Disorder?
Substance use disorders (SUDs) are treatable afflictions characterized by a chronic pattern of substance use. SUDs impair lives in many different ways such as in health, social function, relationships, financial status, self-image, and more.
Substance use disorders start as a voluntary action, a person choosing to take a substance, but over time it develops into something more than that. Depending on the specific substance, things like cravings can keep them in the loop of substance use. In other instances, untreated mental health and other outside factors can play a large role both in the start of an SUD as well as the continuation of it.
It has been observed that around half of those experiencing substance use disorder have a co-occurring mental health condition.
You may hear of SUDs referred to as “addiction” but we tend to discourage the use of that terminology. The term “addiction” relates heavily to the word “addict” which often implies that the person is the “problem” rather than being a person who is dealing with a “problem.”
Something important to remember is that the cause of substance use disorder is complicated and there is not a simple formula that can get to the root of why a person may have an SUD. Many factors may need to be addressed to help your loved one make a successful recovery.
What Are the Common Signs of a Substance Use Disorder?
Cravings – A person experiencing substance use disorder often has intense cravings for the substance that they have been taking. You may find that your loved one is unlike themselves until they can satisfy this craving. As substance use continues, their priorities might shift completely to fulfilling these cravings.
Dependence – If a person is experiencing dependence, their body has become used to having the substance. If this person stops their substance use their body will experience physical symptoms due to the absence of the substance.
Tolerance – If someone is taking more of a substance to feel the same effects that they once felt, their body has built up a tolerance to the substance. This means that the body has become used to the presence of the substance and requires more of the substance to achieve the same results. This contributes to the reasons a person might progressively use higher doses of a substance.
Withdrawal Symptoms – The physical and mental symptoms that occur when someone stops taking a substance they’ve regularly partaken in are called withdrawal symptoms. These occur because the body is adjusting to no longer having the substance or substances within the body.
Poor Judgment – If your loved one is managing a substance use disorder, it may seem as if they demonstrate a lack of judgment. Because of the intense cravings that they have for a substance, they may start to use unsafe methods to pursue these cravings.
Financial Issues – A significant sign of a substance use disorder is the presence of financial issues. A person may use up their financial resources in pursuit of their substance use and start taking extreme measures to gain extra money.
What Are the Most Common Substances for SUDs?
While there is nearly an infinite number of combinations of substances that can contribute to a substance use disorder, statistics show what substances are most commonly treated at recovery facilities. The highest-ranking ones include alcohol, pain relievers, methamphetamine, cocaine, heroin, and other illicit drugs.
As you seek treatment for your child, we encourage you to speak with qualified professionals who have experience treating substance use disorder so that you can be sure that you are taking the appropriate steps to support your child in their recovery.
Alcohol
Alcohol is the most common substance involved in substance use disorders. This is often referred to as an alcohol use disorder (AUD) or “alcoholism.” Much like the term “addiction,” alcoholism also has a stigma tied to it.
Because it is legal to consume, alcohol becomes a common substance of choice. Both during self-discovery phases and during times of mental turmoil, alcohol can act like a bandaid. Consistent consumption of alcohol can lead to an AUD and alcohol withdrawal. Long-term effects of alcohol use include high blood pressure, heart disease, increased potential for stroke, increased risk of cancer, weakening of the immune system, learning and memory problems, increased risk of mental health problems, and increased likelihood of social problems.
Pain Relievers/Opioids
Prescription pain relievers, especially opioids, are often seen in the world of substance use. Opioids are an increasingly common substance, but fentanyl in particular is gaining widespread use due to its cheap cost and powerful effects. Other examples of opioids include codeine, oxycodone, morphine, and methadone. Many opioids were developed as strong pain relievers that work by binding to receptors within the brain, decreasing the body’s perception of pain and elevating a person’s mood by increasing the body’s level of dopamine.
Opioids impact the body’s natural chemical reward system, affecting a person’s decision-making ability. Due to how our bodies process opioids, the withdrawal process can involve intense cravings and side effects. Loved ones will need support as they start their recovery journey. Different medications exist that can assist those with substance use disorder as they recover from their opioid use. These medications will be discussed in greater detail when we discuss treatment modalities in Chapter 4.
Methamphetamine
Methamphetamine, commonly referred to as meth, works by increasing the amount of dopamine that a person’s brain produces. Someone using this substance will experience increased energy, the ability to do more physical activity, decreased appetite, faster breathing, a rapid and irregular heartbeat, and increased blood pressure and body temperature. Long-term methamphetamine use can produce extreme weight loss, dental problems, intense itching that produces sores, anxiety, confusion, memory loss, insomnia, paranoid behavior, and hallucinations.
Cocaine
Cocaine is a substance that works by binding to the brain’s dopamine transporter, blocking the removal of dopamine from the synapse. This is what causes the euphoria commonly experienced immediately after taking cocaine. Cocaine also increases the levels of serotonin present in a person. This hormone helps to stabilize a person’s mood, regulates feelings of well-being and happiness, regulates anxiety, and controls sleep. It also creates feelings of euphoria, high energy, extreme alertness, sensitivity to physical stimuli, and a decreased need for food and sleep.
With regular use, tolerance may develop so that more frequent and higher doses of cocaine are needed to produce the same level of pleasure and relief from withdrawal experienced initially. As tolerance to cocaine builds, a person becomes more susceptible to overdose as they continue to increase the dosage of the substance to try and achieve the desired effect.
Heroin
Heroin is a common example of an opioid. Unlike other forms of opioids, however, heroin is strictly illicit. There isn’t a form of heroin used in the medical field. Because of this, heroin has a much higher chance of having unknown ingredients mixed or laced with it. This increases the risks involved with heroin consumption, though no form of illicit substance use is risk-free.
Just like other forms of opioids, heroin overdoses pose a risk of serious injury or death. When taking the steps away from heroin, intense cravings and other withdrawal symptoms can make the task seem harder than it is. This is where medical detox programs can come into play.
Other Illicit Drugs/Benzodiazepines
Other forms of illicit drugs include anything that is illegal or is being taken without direction from a doctor. One such medication that is often seen in this regard is benzodiazepine. Benzodiazepines are a type of substance developed to treat anxiety, insomnia, and seizures. Examples of this medication include Klonopin, Xanax, and Valium. Benzodiazepines work by suppressing certain nerves in the brain that are believed to be associated with anxiety. They also cause a surge of dopamine in the brain causing intense feelings of pleasure for the person using benzodiazepines.
A particular danger related to benzodiazepine use is that many take them alongside other substances. For example, someone might mix a benzodiazepine with an opioid to create enhanced euphoric effects. In this case, a person will also experience the dangers of both substances. This can greatly increase a person’s risk of experiencing a fatal overdose.
A final important note is that benzodiazepines are extremely dangerous to detox from alone. Serious medical and psychological complications result from going cold turkey. To find recovery from a benzo use disorder, one must seek professional help either through a taper protocol with their doctor or a medical detox at an addiction treatment provider.
Chapter 2: What Causes Substance Use Disorders?
In Chapter 1 we briefly mentioned that the causes behind substance use disorders can be complex and often can’t be reduced to one simple problem. Many factors can contribute to a person developing a substance use disorder. Below are the most significant contributing factors to SUDs. As you read through these factors, take some time to think about how all of these components could contribute to your child’s situation.
How Substance Use Affects the Brain
When a person engages in substance use, they are putting a chemical into their body that affects their brain. Some substances, such as marijuana or heroin, do this by mimicking our body’s neurotransmitters. This causes these neurotransmitters to receive abnormal messages from the substances. Others, such as cocaine or methamphetamine, cause nerve cells to release excessive dopamine, or prevent the normal recycling of dopamine.
A good way to think about how substances affect the brain is that the substance provides a shortcut to receiving the chemicals that the brain naturally releases during moments of pleasure. Many substances take control of this system of dopamine release. Dopamine does not cause the rush of feelings, but it does reinforce the desire to use substances.
Additionally, over time the continued presence of substances in a person’s system leads to the brain becoming accustomed to how they alter our body’s functions. This can lead to a feeling of need whenever the substance isn’t present because our body thinks the substance is required to function properly.
Genetic Factors
Many people believe that genetics play a determining role in whether or not a person develops a substance use disorder. While some evidence exists highlighting the role that genetics play in substance use disorder, there has been no single genetic factor discovered that distinguishes between those who develop a substance use disorder, and those who have tried substances but never developed an SUD. On a practical level, this means that substance use disorder is not a predetermined and unbeatable condition. Instead, it is a condition caused by many complex factors that can be treated and overcome with the correct support system.
Other Mental Health Issues and Trauma
In Chapter 1 we mentioned that it is common for someone with substance use disorder to have a co-occurring mental health condition. This does not necessarily mean that substance use causes mental health issues. It also does not mean that mental health issues cause substance use disorder. What it does mean is that there is a complex interplay occurring between mental health and substance use.
Sometimes a person with a mental health condition starts using a substance in an attempt to self-medicate. Other times substance use may affect a person’s brain structure and lay the foundation for a mental health condition. In some cases, because mental health conditions and substance use disorder share many of the same risk factors, there is no clear answer on which came first or caused the other.
What is clear is that substance use and poor mental health often go hand in hand. Working through a person’s mental health, including work to understand and process traumatic life events, will likely be part of treating your child’s substance use disorder.
Social Environment
Social environment is an important factor in the development of substance use disorder. A person is much more likely to engage in substance use if their primary social circle does. You may have even experienced this yourself. Many people who only drink alcohol occasionally describe themselves as “social drinkers.” This means that it is fairly uncommon for a person to drink alcohol, and when they do, it is usually in a social setting where most other people present are also drinking alcohol. Being a social drinker is a very mild example of how a social environment can affect a person’s substance use.
If your loved one is friends with people who bond by engaging in substance use, they will likely also try out or regularly consume the same substances. Substance use can bring with it a sense of belonging to the group. It is very common for young people to move through a phase of experimentation with substance use with their friends. Often this phase resolves itself naturally, but for some people, substance use becomes their primary social activity making them seek out others who have chosen to do the same. The establishment of a support network filled with people who encourage healthy behaviors will be an important factor as your child continues to recover from substance use disorder.
Role of Family
As uncomfortable as it is to consider, the families of those who develop a substance use disorder must make an honest assessment of how they may have contributed to their child’s substance use. This is not a time for blame or shame, but an opportunity to consider what family behaviors could have contributed to your child’s substance use and how you can be part of their recovery solution. Remember, just because a traumatic family event may have contributed to a person’s decision to seek comfort with substance use, it does not mean that you are responsible. All families face challenges that are often complex and everyone is on a journey to learn how to manage difficult situations and feelings healthily.
One thing to consider is your own family’s substance use. It is 37% more likely that a person will develop a substance use disorder if they had a parent who also had an SUD. The norms laid out by parents are a large contributing factor to SUDs.
It is also possible that families contribute to substance use less directly. If a family unit experiences an unhealthy amount of conflict, this could cause someone to seek relief through substance use.
Substance use affects the whole family. You as a parent may be hurting because your child stole money or lied to you. They may be hurting because of a traumatic event that caused them to seek relief through substance use. Maybe there are siblings in the mix who just miss the relationship they used to have with their brother or sister. Substance use disorder is a wake-up call for families. It lets them know that it is time to seek help and address issues that have caused harm to the family, and find new tools to help them communicate, support, and love one another.
Failure to Launch
An increasingly common issue that young people face has been unofficially labeled as “failure to launch.” This describes a young person who has difficulties transitioning into becoming independent when they reach adulthood. Failure to launch takes on many different faces. Maybe your adult child never had the motivation to pursue additional education after graduation and they are content with living in your home while working a part-time, minimum-wage job. Maybe your child went to college and got a degree, but could not secure a job in their field of study and needed to return home. It is also possible that your child was able to move out and secure some level of independence but you are still somewhat financially responsible for their well-being by paying their rent or assisting them with a car payment.
It is tempting to offer dismissive explanations as to why young people fail to launch into adulthood. It is true that lazy and entitled people exist in every generation, but the issues driving failure to launch go deeper than a poor work ethic or the need for a new perspective on their place in the world. Many young people experience a significant financial burden due to factors beyond their control as they enter adulthood. Others might point out that the increased protectiveness of parents created young adults who are simply not ready to face the challenges of independent living. Finally, the increase in mental health issues is a factor in the inability of young people to move into an independent stage of life. Just like substance use disorders, failure to launch cannot be oversimplified and is often based on the intersection of numerous complex factors.
Failure to launch is often present alongside substance use disorder because both have many of the same drivers. For example, a person who is experiencing extreme anxiety may not be able to live independently due to the anxiety, and may also seek out substances to decrease the amount of anxiety that they feel. You can see that in this example the root cause of both challenges is the anxiety, not the substance use or the failure to launch. If your adult child is experiencing failure to launch alongside a substance use disorder, a trained counselor will be able to guide you both in creating the right environment for increased independence and recovery from substance use.
Chapter 3: Withdrawal
Withdrawal is the name for the process of a person’s body adjusting to functioning without substances being present. Because these substances produce various effects within the body, a person’s body must re-learn how to do its usual functions without the presence of the substance.
Withdrawal symptoms can be difficult for the person who is experiencing them, and difficult for you as their parent as you support them through their recovery. The good news is that withdrawal is not forever and a person can endure the unpleasant symptoms and find recovery on the other side. Below are some descriptions of the common withdrawal experiences based on different substances so you can know what to expect as you support your child in their recovery.
Opioids
Opioid withdrawal symptoms generally mimic a bad flu while also including symptoms such as agitation and anxiety. These symptoms will likely start around 12 hours after the dose was taken and the worst of the symptoms will likely last from 24-48 hours. Some mild symptoms can linger for weeks or months but typically symptoms are over after a few days.
Some people experience diarrhea or vomiting to the extent that death by dehydration is possible. Also, because opioids lower a person’s blood pressure, heart rate, and respiratory rate, it is possible that a person could suffer a heart attack or stroke if their vital signs increase too quickly during withdrawal. The primary concern regarding opioid withdrawal, however, stems from the cravings that commonly accompany it.
Cravings are the biggest risk of withdrawal. Cravings for opioids can sometimes last months. This is why it is recommended that someone detoxing from opioid use do so under the supervision of medical professionals. There are options and medications available to make this period safer and easier.
Cocaine
Because cocaine acts as a powerful stimulant, the first symptom of cocaine withdrawal is significant physical fatigue. A person detoxing from cocaine will likely also experience cravings, depression, anxiety, paranoia, insomnia, and nightmares. These symptoms usually last from 7-10 days. However, cravings often last for much longer and cravings can resurface years after a person has last used cocaine.
Withdrawal cravings are intense for someone in the detox phase of recovery from cocaine. A support system must be in place as your child continues their detox because it is common for those detoxing from cocaine to return to cocaine to achieve relief from these cravings and other symptoms.
Alcohol
Alcohol withdrawal symptoms will vary in severity depending on how long a person has been drinking and the amount of alcohol that they have been consuming. Someone who has a serious alcohol use disorder will likely start their withdrawal symptoms around 6 hours after their last drink. The early symptoms that they will feel include anxiety, shaky hands, headache, nausea, vomiting, insomnia, and sweating. Some who consumed alcohol more heavily might experience hallucinations or seizures within the first two days of starting an alcohol detox. Rare symptoms present in those who have used a very heavy amount of alcohol include vivid hallucinations and delusions from 48-72 hours after detox starts. This only happens in around 5% of those who detox from alcohol.
The worst symptoms of alcohol withdrawal typically end after 72 hours. Some symptoms can linger for around 5 weeks. It is common to experience cravings and emotional effects related to alcohol use after detox is complete, so forethought into support for your child as they recover is a wise course of action.
Benzodiazepines
The average benzodiazepine withdrawal timeline is 3 to 4 days after the last dose of benzodiazepine was taken. Occasionally benzodiazepine withdrawal starts with a few mild symptoms that are present for a few days, such as disturbed sleep or agitation, with other symptoms such as anxiety, restlessness, hand tremors, racing pulse, panic attacks, or blurred vision developing as withdrawal continues. Somewhere between 10 and 25 percent of those who have a benzo use disorder will experience protracted withdrawal, which is when a person experiences withdrawal symptoms off and on for several months following their last use of a benzodiazepine.
Remember, serious medical and psychological complications result from going cold turkey. When a person detoxes from benzos it is best if they seek out professional help to manage the withdrawal symptoms safely.
Methamphetamine
Those with a methamphetamine use disorder often enter withdrawal in a weakened state. This is because of the extreme toll meth can take on a person’s body throughout their history of substance use. The symptoms of methamphetamine withdrawal include an extreme lack of energy, sleeping too much, psychosis, anxiety, paranoia, and depression.
Someone withdrawing from methamphetamine use can expect to sleep for nearly 24 hours a day for one week due to an extreme lack of energy. The depression that results from a methamphetamine withdrawal can be very long-lasting, and cravings following the withdrawal can continue to be very strong. The good news is that methamphetamine withdrawal does not have the potentially fatal effects associated with other drugs.
Don’t Forget Your Compassion -- Withdrawal Is Hard
As you can see, the task of detoxing from a substance can seem daunting for someone experiencing substance use disorder. They may feel at times that it is not worth the symptoms and hardship that accompany the period of withdrawal. This is normal and is a time to be empathetic for your child as they set out to accomplish a difficult part of their recovery journey. You might recall a time in your own life when you set out to reduce your caffeine intake, eat a more balanced diet, or exercise more regularly. Those tasks may have been difficult without the more intense symptoms associated with detoxing from a harmful substance.
During this time, remember to continue to support your child, and rely on the insight of trained professionals who have helped many through this process before. The detox period of recovery is uncomfortable for most, but it is not only possible, it is common for those who get the proper support to make it through the detox period and recover from their substance use disorder.
Chapter 4: Treatment Modalities and Medications
A treatment modality is simply a method of treatment, in this case specifically for substance use disorders. There are many different kinds of treatments and it is important to work with treatment providers to choose the mode that will best serve your loved one. Not all treatments work for everyone but with the variety of treatment options available, there is a high likelihood that a compatible treatment exists for your child.
If you do not have a clinical background it may seem overwhelming to look at all these different treatment options! You might also feel a sense of anxiety, wondering if it is possible to choose the wrong treatment option for your child as they start their recovery journey.
This is why it is always best to discuss treatment options with a licensed clinician. They can help you figure out the best treatments for your loved one. Remember, many of these treatments work well when paired together. The support found in a 12-step group can complement the evidence-based practices of cognitive behavioral therapy while greater emotional awareness is fostered through art therapy. Be sure to have involved conversations between yourself, your family, your clinician, and your child who is seeking recovery for their substance use disorder.
12-Step Programs
12-step programs are based on a philosophy that 12 consecutive activities, or steps, should be completed during the recovery process. These steps often include admitting powerlessness over alcohol and drugs, taking a moral inventory of themselves, admitting the nature of their wrongs, making a list of individuals whom they have harmed, and making amends to those people.
12-step groups are meant to provide participants with support for remaining substance-free via people who understand the recovery process, and a guideline that a person can live by as they pursue recovery. 12-step programs can and have worked for individuals from a variety of backgrounds, but they tend to be much more effective for those coming from a background where their faith is, or at one time was, important to them.
Motivational Interviewing and Motivational Enhancement
Motivational Interviewing (MI) is a person-centered clinical method often used when a client is reluctant or apathetic about their ability to change. MI seeks to discover the client’s motivations, strengths, and resources. This method is specifically designed to strengthen a client's motivation for and commitment to positive change. When exploring the possibilities of change, particular attention is paid to the way a person speaks to predict subsequent change. The therapist explores the client’s reasons for change within an atmosphere of acceptance to minimize resistance and defensiveness.
Motivational Enhancement combines the style of motivational interviewing with individual assessment feedback that may be particularly helpful for people who are hesitant about their recovery journey.
In both Motivational Interviewing and Motivational Enhancement, a person works toward a goal only when they indicate that they are ready. The therapist does not set the goal, they empathetically listen until the person indicates what their goal is and then the therapist helps them to meet that goal. Total abstinence may not be a person’s goal, but the therapist will work with the person to give them the tools they need to reach the goal they set for themselves.
Cognitive Behavioral Therapy
During Cognitive Behavioral Therapy or CBT, a person works with a mental health counselor in a structured way. CBT helps a person become aware of inaccurate or negative thinking so they can start to think about challenging situations with more clarity and respond to them more effectively. CBT has been proven to be effective at treating several conditions including substance use disorders, depression, anxiety, marital problems, eating disorders, and severe mental illness.
Someone participating in CBT as part of their treatment will have to confront aspects of their life that they would rather ignore, sometimes leading to them feeling physically or emotionally drained after a session. It is a good practice to schedule time for a person to process what they have worked through during their therapy session. Often cognitive behavioral therapy can help your child understand the root causes of their substance use disorder and how to address those causes in positive ways.
Rational Emotional Behavior Therapy
Rational Emotive Behavior Therapy, or REBT, is a form of therapy that helps a person identify self-defeating thoughts and feelings, challenge those attitudes, and replace them with healthier, more productive thoughts and feelings. REBT can help a person work through difficult emotions such as anxiety, depression, guilt, and anger. This approach is also used to help change stressful and self-defeating behaviors, such as aggression, substance use, unhealthy eating, and procrastination so that a person can overcome their obstacles and achieve their goals.
REBT is different from other cognitive-behavioral approaches by emphasizing the contrast between irrational and rational beliefs. In REBT rational beliefs have characteristics such as being flexible, non-extreme, and logical, and in contrast, irrational beliefs are described as rigid, extreme, and illogical. REBT seeks to help a person accept beliefs that are rational and helpful, while also letting go of beliefs that hold the person back.
Dialectical Behavioral Therapy
Dialectical Behavioral Therapy, also known as DBT, was originally developed to treat borderline personality disorder. Over time it has become clear that DBT is a successful treatment for people experiencing depression, bulimia, binge eating, bipolar disorder, post-traumatic stress disorder, and substance use. DBT skills are ideal for those who wish to improve their ability to regulate emotions, endure distress and negative emotions, be mindful and present in the given moment, and communicate and interact effectively with others.
During DBT a therapist helps a person learn skills in four key areas. The first area is mindfulness, which helps a person focus on accepting and being present in the current moment. Second, a person learns to increase their tolerance of negative emotion, rather than trying to escape from it. Third, a person works on emotional regulation, which covers strategies to manage intense emotions that are causing problems in a person’s life. The fourth skill is interpersonal effectiveness, which consists of techniques that allow a person to communicate with assertiveness, self-respect, and to strengthen relationships.
Eye Movement Desensitization and Reprocessing
Eye Movement Desensitization and Reprocessing, or EMDR, is a fairly new therapeutic approach that was developed to treat individuals with post-traumatic stress disorder. It’s traditional exposure therapy combined with a focus on eye movements that signal various aspects of trauma. During EMDR a person’s own rapid, rhythmic eye movements dampen the power of emotionally charged memories of past traumatic events. Along with PTSD, EMDR has shown success in treating substance use, panic attacks, eating disorders, and anxiety.
During EMDR, a therapist will move their fingers back and forth in front of a person’s face and ask them to follow hand motions with their eyes. While doing this, the therapist will have a person recall a disturbing event. This will include the emotions and body sensations that go along with it. Gradually, the therapist will guide a person to shift their thoughts to more pleasant ones. This method may sound unconventional at first, but therapists who practice EMDR say that this method of treatment can weaken the distress caused by disturbing memories.
Seeking Safety
Seeking Safety is a therapeutic approach designed to help a person envision what safety would look like and feel like in their lives, then help them find new ways of coping as well as grounding techniques. One of the goals of seeking safety is to focus on ideals to counter their previous loss through both trauma and substance use. Another objective is to help the client attain safety in their thinking, emotions, behaviors, and relationships. The seeking safety approach could be summarized as a therapeutic approach that will help a person feel safe, empowering them to take control of their life and move in a positive direction.
Family-Assisted Therapy
Family-assisted therapy is an approach that can help improve relationships between family members. Because substance use disorders often have roots in the trauma that someone has experienced, it is beneficial for families to meet with a mental health professional to work through any issues that may be related to a person’s substance use.
Family therapy is useful for helping work through situations that cause stress, grief, anger, or conflict. It can increase your family members' communication skills, and understanding of one another better and teach family members coping skills to bring everyone closer together.
Psychodynamic
Psychodynamic therapy is an approach that is primarily used to treat depression and other serious mental health disorders. This method is also useful in treating social anxiety disorder, eating disorders, problems with pain, relationship difficulties, and substance use disorder.
During psychodynamic therapy, a person will work with a therapist and learn to speak freely about anything that comes to mind. Common topics include current difficulties, fears, desires, dreams, and fantasies. The goal is to minimize symptoms that lead to harm, and also lead to positive changes like increased self-worth, better use of a person’s talents and abilities, and an improved capacity for developing and maintaining more satisfying relationships.
Holistic Psychotherapy
Holistic psychotherapy is an integrative approach that focuses on the relationship between a person’s mind, body, and spirit. This method attempts to understand and address the ways issues in one aspect of a person’s life can lead to concerns in other areas.
In holistic approaches, a person learns how all aspects of their health and wellness are connected and focuses on how a person can experience increased health and wellness by acknowledging and addressing this interconnectedness. These approaches are useful in treating anxiety, depression, substance use, and stress, and can be helpful to someone processing traumatic life events.
Dual Diagnosis & Co-occurring Disorders
In the past, mental health treatment and substance use disorder treatment were treated as two separate issues with separate approaches. Dual diagnosis or co-occurring disorder means that the two separate issues that a person has are addressed and treated at the same time. It is common for substance use disorders to complicate a person’s mental health condition, and it is also common for substance use to have roots in a person’s mental health issues. Dual diagnosis seeks to treat both SUDs and mental health with special attention paid to the ways that they intersect and affect each other.
Trauma-Informed Care
Trauma-informed care is an approach that seeks to understand a whole person. In trauma-informed care, it is assumed that the person seeking treatment for mental health or substance use disorder probably does have some sort of trauma in their background that is the root of the presenting issues. Trauma-informed care seeks to understand the root cause of why a person seeks treatment, not just to treat the symptoms. A good way to think about trauma-informed care is that instead of asking “What is wrong with you?” it asks “What happened to you?”
Art and Music Therapy
Art and Music Therapy are valuable tools in a person’s recovery journey that can complement evidence-based therapeutic practices. Music and art are helpful to a person as they seek to manage anxiety and reconnect with their emotions. It even helps a person’s brain recover from damage caused by sustained substance use. As a person seeks to occupy themselves after substance use ends, art or music could be part of what gives a person's life meaning. Creative practices such as art and music are helpful tools to manage emotion, and for many are a great alternative to substance use.
As we mentioned in our section on Motivational Interviewing, motivation is a key component in an individual’s recovery. While extracurricular therapies may not have specific evidence-based effects, when integrated into overall therapy models, they can help attract and retain interest in the recovery process.
Medication’s Involvement with Treatment
Many different medications play a role in the recovery from substance use. This ranges from medications designed to assist with withdrawal, to mental health assistant medication, to medication that can save someone’s life in the event of an overdose. While you do not need to memorize these, and you may not encounter all of them, having a general understanding can help when moving through the recovery process.
Antidepressants
Antidepressants are a medication that can help a person as they seek treatment for depression, which is often a contributing factor to substance use disorder. Typically an antidepressant is used alongside therapy to treat a person’s depression. Antidepressants work by adjusting a person’s neurotransmitters. It is important to stay in contact with healthcare providers while taking an antidepressant. Many can be habit-forming when not taken correctly and could lead to further substance use issues. Under the supervision of a healthcare professional, and alongside a treatment, antidepressants can be a useful tool for a person seeking to overcome the contributing factors that led to their substance use disorder.
Naltrexone (Prescription Name: Vivitrol)
Naltrexone is a medication that is used to treat those in recovery from alcohol or opioid use. It causes a person to decrease the amount of alcohol that they crave. When treating those in recovery from opioid use, Naltrexone prevents opioids from attaching to neurochemical centers in the brain, which prevents the opioid from having its usual effects on a person. To simplify, with either substance, Naltrexone decreases the pleasurable feelings associated with taking the substance, giving the person in recovery less incentive to use the substance.
It is important to wait until after detox for an opioid user to take Naltrexone. If a person takes the medication while opioids are still in their system it will cause sudden and severe withdrawal symptoms.
Acamprosate
Acamprosate is a medication that works to treat alcohol use disorder. Acamprosate works by decreasing a person’s urge to use alcohol. Acamprosate does not help with symptoms of alcohol withdrawal.
One benefit of acamprosate is that it works to rebalance the neurotransmitters in a person’s brain that has been disrupted by alcohol. Another benefit is that acamprosate does not react with other medications, making it a useful choice for those who are working through a co-occurring disorder.
Buprenorphine (Prescription Names: Suboxone, Subutex)
Buprenorphine is a medication used to treat opioid use. As with all medications used, buprenorphine should be prescribed by a healthcare professional who can monitor and adjust its use as needed. Buprenorphine can be prescribed or dispensed in physician offices, significantly increasing access to the treatment.
Buprenorphine works by occupying the brain’s receptors without producing the pleasurable effects of opioid use. If a person attempts to take an opioid while on buprenorphine, they will not experience the euphoria normally associated with opioid use. Buprenorphine can be habit-forming when not taken as directed so it is always important to follow a physician’s instructions when using the medication.
There are three common types of Buprenorphine: Suboxone, Subutex, and Sublocade. Suboxone has been used in addiction treatment since 2002 and is taken orally every day. Sublocade was introduced and approved in 2017. Sublocade is a once-a-month injection that a person can receive from a healthcare professional. Subutex is an oral medication much like Suboxone. The difference between these two medications is that Suboxone has naloxone added to it, which helps prevent the medication from becoming addictive.
Chapter 5: Arizona Certification for Treatment Centers
JCAHO
The Joint Commission on Accreditation of Healthcare Organizations, or JCAHO, is a nonprofit organization based in the United States that accredits healthcare organizations and programs throughout the country. Often JCAHO is simply referred to as the Joint Commission by those who work in the healthcare industry. Joint Commission accreditation standards are designed to help improve the quality of care received by patients. JCAHO standards will help an organization manage and reduce the risk of error or low-quality care.
The Joint Commission develops standards that are developed by experts in their field, and periodically these standards are put up for field review. JCAHO accredits hospitals, home health care providers, nursing homes, behavioral health centers, ambulatory care centers, and laboratory services. A Joint Commission-accredited facility means that the facility has gone through a lengthy process to prove that it provides high-quality care.
CARF
CARF stands for the Commission on Accreditation of Rehabilitation Facilities. CARF’s offices are located in Tucson, Arizona. CARF is an independent, nonprofit accreditor of health and human services. CARF provides accreditation in the areas of Behavioral Health, Child and Youth Services, Opioid Treatment Programs, Aging Services, Durable Medical Equipment, Employment and Community Services, Medical Rehabilitation, and Vision Rehabilitation Services. CARF applies sets of quality standards during a consultation with a provider. This consultation takes place on-site at the treatment facility. The result is that this consultation process helps providers in improving the quality of their services.
Being CARF accredited means that a facility has gone through its accreditation process and has met its high standards for patient care. Knowing that a facility is CARF accredited means that you know they have been approved by an independent source to provide life-saving services to your loved ones.
Chapter 6: Continuum of Care
The continuum of care is the idea that for many conditions, including substance use disorder, care does not end with the initial treatment but instead evolves.
As a person makes progress along their road to recovery the need for detox and inpatient treatment will fade and both individual and community support will take their places to promote a healthy life free of substance use. Below are some common stages of the recovery process, but remember that everyone is different. These stages are more of a guideline of what you might experience and less of a formula that will tell you exactly what will happen.
Stage 1 — Treatment Engagement
During stage 1, a person’s care team determines the extent of impact concerning substance use on physical, psychological, and social levels. The care team also evaluates a person’s social support network as part of developing their treatment plan. The counselor explains program rules and expectations and works to stabilize any crises. This stage will include the detox stage when the person feels most in crisis.
One of the dangers of this stage of treatment is that it is often the most difficult and a person in recovery will be tempted to quit so one of the most important tasks during this stage is to foster commitment to the program for the person in recovery. This stage typically lasts from a few days to a few weeks and focuses on the following goals:
- Completed withdrawal from substance use
- Resolved any immediate crises
- Completed orientation to the recovery program
- Established a treatment plan with treatment providers
- Attended scheduled sessions regularly
- Completed the assessment process
Stage 2 — Early Recovery
Stage 2 is highly structured with educational opportunities, group involvement, and the introduction of new behaviors to help a person develop the skills they need to build a life in recovery and address potential lapses. The early recovery stage will likely involve inpatient care or intensive outpatient care.
Early recovery involves the end of the detox stage and likely transition into a residential treatment program where a person will learn skills to continue their recovery. Early recovery lasts from 6 weeks to 3 months and includes the following goals:
- Abstinence from substance use for 30 days or longer
- Completed goals as indicated in the treatment plan
- Created and implemented a plan for relapse prevention and continuing care
- Regular support group participation
- Maintained a substance-free social support network
- Obtained stable, substance-free housing
- Resolved any situations that may trigger relapse
Stage 3 — Maintenance
Doing effective treatment in a continuum of care means that, over time, care will become less intensive, and contact with treatment staff will taper off. This is what occurs during the maintenance stage. A person and their care team must prepare for the transition to less intensive treatment. This transition to less intensive forms of care is a transition that must be approached with care. Removal of support too soon can lead to relapse.
Often the care received during stage 3 can be provided by the same staff and in the same facility. In other cases, a person receives care through a different facility specializing in a transitional care period. The maintenance stage typically lasts from 2 months to one year. The goals of the maintenance stage are as follows:
- Solidify recovery
- Practice relapse prevention skills
- Improve emotional health
- Broaden supportive social networks
- Address problem areas
Stage 4 — Community Support
When a person is discharged from formal treatment to continuing community support, they are committing to a lifestyle of continued recovery. People who remain within a system of ongoing care relevant to their needs are more likely to maintain their gains in recovery and overall lifestyle changes. The community care stage is ongoing. Someone in recovery should always be attentive to the support that they need to continue to live a healthy lifestyle.
So what does the community support stage look like? This is to be determined by the person who is in recovery from substance use and their loved ones. Some common practices include attending a 12-step or other recovery support group, participation in a spiritual community, continued meeting with a therapist, practices that help them connect with their emotions, a renewed focus on health and wellness, and simply being in a community with people that encourage them to continue in recovery.
Chapter 7: Life in Recovery
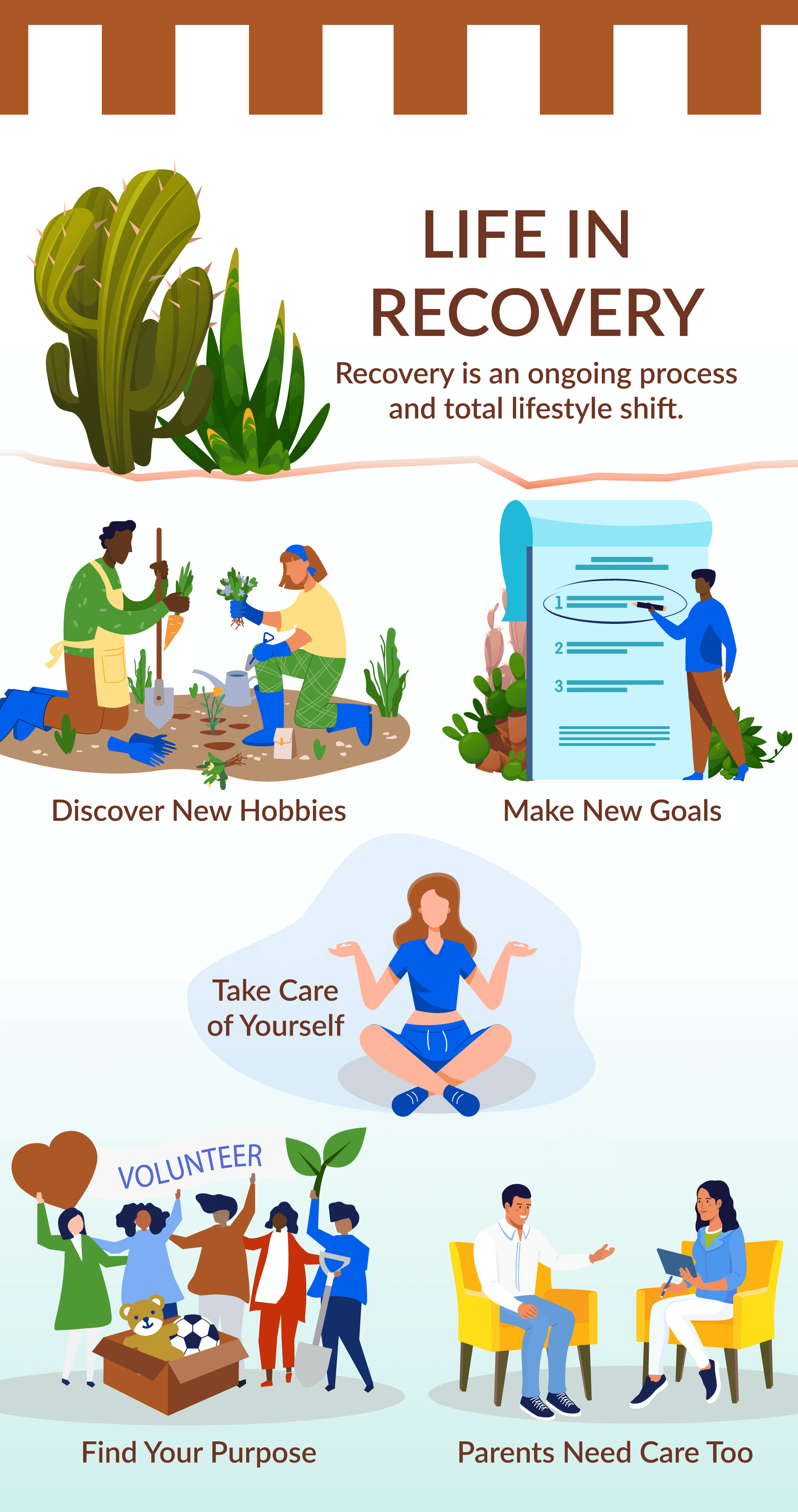
As stated in Chapter 6, recovery is an ongoing process and a total lifestyle shift. A person has the opportunity to explore new ways of living and discover what helps them to be mentally, physically, spiritually, and emotionally healthy.
Discover New Hobbies
Often a person’s list of activities and social circle diminish after recovery. If someone’s life revolved around their substance of choice before recovery, their social circles are likely no longer healthy for them. Often, those in recovery find new hobbies that improve their overall well-being. Some might do yoga or participate in organized sports. Others might take up a fitness practice. Some may choose to engage in a creative hobby, while others may do something that involves spending time in nature. Hobbies, activities, and new community connections are important to a person in recovery. Stopping unhealthy practices is not enough, a person must replace them with healthy practices that contribute to overall wellness.
Make New Goals
In formal treatment, a person will get used to making goals related to their recovery. A good practice is to continue to make goals. Achieving these goals will give a person in recovery the motivation that they need to continue to make healthy choices that support their recovery.
The goals do not necessarily have to be about recovery in every instance. For example, a person could make it a goal to read one book a month. Similarly, if they started a fitness goal, they could make it a goal to achieve a new level of fitness by running farther or lifting more than they have previously managed. A person looking for new community connections could even make it a goal to attend three new social events in a month. Goals that contribute to overall health and happiness should be encouraged as your child discovers what their new life looks like.
Take Care of Yourself
The standard health advice that your doctor tells everyone also applies to people in recovery! Eating right, exercising, and getting enough sleep are important practices for someone who is healing from the effects of substance use. An important truth to remember is that substance use damages the mind and body, but healthy practices can help a person heal and experience wholeness.
Healthy practices can factor into a person’s goal setting mentioned above. Maybe a person can try a new healthy recipe every week. Another option would be to set a goal to eat dessert less often (but of course not never!) Health goals can help a person take control of their life and own their recovery journey.
Find Your Purpose
Everyone is looking for some kind of purpose. As a person settles into their recovery journey, they may start to look outward for meaning. Participation in communities can be very meaningful for someone in recovery. In a community, people find value in being part of something bigger than themselves. A community that centers around love and acceptance where all people are treated as if they are important can be a great support system for someone in recovery, and they can participate in being a support to others they are in the community with.
Volunteering might also be a great way to find purpose. Sometimes those who’ve dealt with substance use feel that they are worthless, but participating in activities that give back to others is tangible evidence of a person’s value!
Parents Need Care, Too
Remember, as you work to support your child through their substance use disorder, you will also need support. It can be distressing to watch someone you love have setbacks, while you only want the best for them. Many of the techniques we talk about that will be helpful for your child may also be helpful for you. You should make sure that your support system is filled with people who can be a presence of hope as you navigate what comes next for you, your child, and your family.
This could involve meeting with a therapist who can help you to receive perspective about your child’s substance use disorder and your role in supporting them. It could also mean making sure your body is healthy so that you are at your best when factors beyond your control cause turmoil. Another important resource that helps many people is support groups for parents who have adult children managing a substance use disorder. Examples include Parents of Addicted Loved Ones (PAL,) Nar-Anon, or Al-Anon.
In a support group for parents, you will likely feel less alone. Many parents don’t realize that many others are experiencing the same things you are as they attempt to love and support their child through substance abuse. In this setting, you will be exposed to the experience of the group who may have perspective on your situation. Many parents talk about the tension between loving their child through substance use and avoiding behaviors that enable substance use. In a group setting, you can explore strategies that will help you act in a way that shows compassion without enabling your child. Many parents feel shame that their child is experiencing substance use disorder, but in a support group you can be reminded that you are not alone and that hope is present.
Regardless of the method of care that is most beneficial to you, taking care of your own needs will be vital as you seek to help your child reach a healthier outcome in their recovery journey.
There’s No Wrong Time to Start - Contact Us Today!
If you are ready to learn more about potential care options for your child, please contact us at Pinnacle Peak Recovery Center so that we can serve you and your family as you work together through the challenges of overcoming addiction. To talk to us about our treatment options, call us at 866-377-4761.
Clinical Excellence | Compassionate Care | Family Feel
Glossary of Important Terms
Acamprosate – This is a medication used along with counseling to treat alcohol dependence. It stabilizes the chemical balance in the brain that would otherwise be disrupted by alcohol withdrawal.
Addiction – The condition of being drawn to a particular substance, thing, or activity due to cravings or how it makes one feel.
AL-ANON – A program that offers support for friends and family members of individuals who are managing an alcohol use disorder.
Alcoholics Anonymous – A support group for those with alcohol use disorder. Most known for creating the 12-step program.
Alcohol Use Disorder – A dependence on the consumption of alcoholic liquor or the mental illness and compulsive behavior resulting from alcohol dependency.
Aftercare Planning – This is the process of sitting down with the individual in recovery, the family, and any counselors post-treatment to plan the next steps. It often involves referral to other support services, recommendations for the family, and reminders of what the individual in recovery can do to remain on the path.
Antabuse – This is the name of the prescription drug disulfiram. It is sometimes used in the treatment of alcohol use disorder. Rather than treating alcohol use disorder, Antabuse works on the liver so that certain enzymes are built up, causing anyone drinking alcohol to become violently ill. It’s very uncommon for it to be used within the US for treatment.
Antidepressants – A treatment medication to help those who have mood disorders with depressive symptoms.
Benzodiazepines – Any of a family of minor tranquilizers that act against anxiety and convulsions and produce sedation and muscle relaxation. Some examples include Xanax, Valium, and Librium.
Binge – A short period devoted to indulging in an activity to excessive amounts such as drinking alcohol or eating.
Blackout – A period that the individual can’t remember, often because of heavy substance use.
Biofeedback – A form of therapy that tracks involuntary reactions such as breathing rate and sweating. It’s meant to teach people to be more aware of the various unconscious processes that can help them understand when to use various coping techniques. For example, if a person in recovery experiences a heart rate increase after seeing someone nearby consume alcohol, they learn how to calm their body down and focus on other things.
Buprenorphine – A medication that is given to individuals with substance use disorders to control moderate to severe pain and treat opioid or alcohol dependence.
Chronic Disease – An illness that lasts three months or more and cannot quickly, or at all, be cured by medication. Examples of chronic diseases include heart disease, cancer, chronic respiratory diseases, etc.
Cocaine – A substance derived from coca or prepared synthetically, used as an illegal stimulant and sometimes medicinally as a local anesthetic.
Comedown/Crash – A term used to describe the experience of the initial euphoric effects of a substance or other potentially addictive behavior wearing off.
Co-Occurring Disorder – When an individual has more than one diagnosable mental illness as defined by the DSM V, for example, Bipolar Disorder and Substance Use Disorder.
Continuum of Care – The range of services from detox to post-treatment follow-up. Some centers will provide a full continuum of care under one roof, while others will have different elements in separate buildings or work with partner organizations.
Delirium Tremens (DT) – Severe withdrawal from alcohol which involves shakes, hallucinations, irregular heart rate, and sweating. It normally occurs about 3 days into withdrawal and lasts 2-3 days.
Detox – A process or period in which one abstains from or rids the body of toxic or unhealthy substances.
Diagnostic and Statistical Manual of Mental Disorders (DSM) – Currently in its fifth iteration, referred to as the DSM V, this book defines all symptoms related to a mental illness diagnosis and clarifies what or how many symptoms must be present to provide diagnosis. There is debate within the field as to the importance of the manual, but it is still the most widely regarded diagnostic tool in the US.
Dual Diagnosis – Similar to a co-occurring disorder, it simply means a person is managing more than one mental health issue or substance use disorder as defined by the DSM V.
Emotional Wellbeing – A positive sense of well-being that enables an individual to be able to function in society and meet the demands of everyday life. Someone who is in good mental health.
Evidence-based Treatment (EBT) – This can be any treatment modality grounded in evidence as derived from scientifically rigorous studies. Cognitive Behavioral Therapy and Motivational Interviewing fall under this category.
Failure to Launch Syndrome – A common way to describe a young adult facing difficulties with the transition to adulthood. The inability to leave home and support oneself, regardless of the underlying cause.
Harm Reduction – A set of practical strategies and ideas aimed at reducing negative consequences associated with drug use. It is also a movement for social justice built on belief in, and respect for, the rights of people who use drugs.
Heroin – A highly addictive analgesic substance derived from morphine, often used illicitly as a narcotic producing euphoria.
Healthcare Insurance Portability and Accountability Act (HIPAA) – The law enacted in 1996 states that health information is private and must be protected by providers, particularly with regulations around electronic storage. This act is why you will be asked to sign a document at a healthcare provider stating you understand your rights and whether or not you allow contact through electronic mediums such as email or text.
Inpatient Care (IP) – the care of patients whose condition requires admission to a hospital or treatment facility.
Intervention – The process of having a group of individuals who are ready to confront a person who is addicted to a substance to persuade them to seek professional help.
Marriage and Family Therapist (MFT) – Marriage and Family Therapists treat a variety of mental health disorders, generally with a focus on couples and families. They must have a Master’s degree and complete a certain number of clinical hours to be licensed by the state.
Methadone – A synthetic analgesic medication that is similar to morphine in its effects but longer acting. Usually used as a medication in the treatment of morphine and heroin addiction.
Methamphetamines – A synthetic substance with more rapid and lasting effects than amphetamine, used illegally as a stimulant and as a prescription drug to treat narcolepsy and maintain blood pressure. It is highly addictive and affects the central nervous system.
Naltrexone – A synthetic medication similar to morphine, that blocks opiate receptors in the nervous system and is used mainly to treat those addicted to heroin.
Narcotics Anonymous (NA) – A group of two or more people in recovery from narcotic use who meet regularly at a specific time and place for recovery from addiction. They are also bound by the same principles of the 12-step program.
Outpatient Care (OP) – Also known as ambulatory care, it is care or treatment that does not require an overnight stay in a medical facility. Care may be instead administered in a medical office, treatment center, or hospital.
Pain Killers – A medication or treatment whose purpose is to relieve pain. Also can be highly addictive. Most popular brands include Vicodin, OxyContin, Percocet, and more.
Parents of Addicted Loved Ones (PAL) – A support group of parents helping other parents whose children are experiencing substance use disorder.
Partial Hospitalization Program (PHP) – A structured program of outpatient psychiatric services as an alternative to inpatient psychiatric care. It’s more intense than the care you get in a doctor’s office or therapist’s office. This treatment is provided during the day and does not require overnight stays.
Private Health Information (PHI) – Any information covered under HIPAA that would identify an individual in conjunction with any medical condition or private health information.
Recovery – A process of change through which individuals improve their health and wellness, live self-directed lives, and strive to reach their full potential.
Recovery-Oriented Systems of Care (ROSC) – These are community-wide networks of care, bringing multiple treatment providers and resources together in a way that is person-centered, building on an individual’s, family’s, and community’s resiliencies and strengths. The purpose of such systems of care is to improve health and wellness outcomes for those managing a substance use disorder.
Rehab – A course of treatment for a substance or alcohol use disorder, typically at a residential facility, but can also be through an outpatient program as well.
Relapse/Return to Use – Falling back into a former state, especially the return of symptoms following a recovery. A person who uses a substance after spending time in recovery would be relapsing. Most often, relapse is defined as the use of any substance one previously engaged with, whether or not that use is excessive. In other words, anything other than complete sobriety is considered a relapse under most definitions. However, there is some debate on this currently since this definition does not allow for progress made. Under the total abstinence definition, even a relapse that was significantly improved from the previous would be regarded in the same way, so there is debate as to the value of the definition.
Sobriety – Is the quality or state of being sober. A state of mind when an individual is not affected by drugs, alcohol, or other substances.
Trauma – A deeply distressing or disturbing experience. It is an emotional response to a terrible event in an individual’s life such as an accident, rape, natural disaster, or death of someone close. Shock and denial are typical. sign of a bar or the sound of parents fighting. Understanding one’s triggers and learning skills to cope with them is essential to long-term recovery.
Trauma-Informed Care – Understanding that lived trauma is often at the root of substance use disorder. To conquer substance use, the individual must also work through the traumatic memories and events that caused them to use substances in the first place.
Trigger – Any event or memory that may cause a person to crave a drug and, thereby, relapse. This could be the sign of a bar or the sound of parents fighting. Understanding one’s triggers and learning skills to cope with them is essential to long-term recovery.
Withdrawal – A group of symptoms that occur upon the abrupt discontinuation or decreased intake of medications or addictive substances.
Wrap-Around Care — Support services surrounding treatment or may also refer to other community providers that provide additional life services such as job skills training, further education, family assistance, etc.