
To understand the dangers of mixing prescription Adderall with alcohol consumption, a person needs full education on how and why they are used separately. This will help when considering the combination of the two.

Amphetamine/dextroamphetamine belongs to a class of drugs known as stimulants. It is one of the most commonly prescribed drugs in the United States and one of the most commonly abused.
Why is Adderall prescribed?
It is prescribed after a physician evaluation to treat attention deficit hyperactivity disorder (ADHD). The only other approved use is to treat narcolepsy to help people feel more awake in daytime hours. By increasing the activity levels of serotonin, norepinephrine, and dopamine, Adderall brings the brain down from a state of overstimulation to a state of baseline stimulation (where most people are, to begin with).
Essentially, Adderall helps the brain control its hyper levels and impulses to one more stable, concurrently snapping the person out of the slowness that tends to settle in their mind (attention deficit). A great comparison for understanding is when a teacher loudly claps their hands and students sit up and focus their eyes on the front of the room.
Doctors and pharmacists follow strict measures to make sure the patient is not abusing the medication themselves or illegally sharing or selling their medication. Laws vary by state but generally prescriptions for stimulant medications require regular office visits in a 60-day or 90-day period.
The Drug Enforcement Agency (DEA), which regulates electronic prescriptions, has allowed e-prescribing of medications including stimulants since 2010. This allows safe transferal of encrypted prescriptions to the pharmacy. The DEA did not approve paper fax versions sent to pharmacies before this, therefore patients were required to obtain a hard copy from the doctor’s office for refill purposes. Some offices without the proper equipment still require this method.
Why is Adderall Misused?
Some people who would normally have no medical need for a prescription become reliant upon Adderall. They do this to meet the spiraling demands of day-to-day living, essentially subbing it for a healthy lifestyle that could be managed in more healthful ways.
Unlike a hamster, it’s exhausting for a person to keep running on an unmanageable life wheel. It may seem hard but is physically necessary to determine how to assess priorities, one of which is a proper sleep schedule.
The National Institute of Neurological Disorders and Stroke states getting enough sleep is “as essential to survival as food and water. Without sleep, you can’t form or maintain the pathways in your brain that let you learn and create new memories, and it’s harder to concentrate and respond quickly. Recent findings suggest that sleep plays a housekeeping role that removes toxins in your brain that build up while you are awake.”2
With society being on the go 24/7, something’s gotta give and for some that thing is sleep. To meet other goals and demands, people are desperate enough to go to measures they normally would not.
Still others might notice its effects recreationally and like the high feeling they receive through use.
How Does This Even Happen? The Example of Friends, John and Jackie
Prescription drugs get in the hands of someone not prescribed the medication through a variety of methods and give very different results depending on why it’s taken. Pain medications are taken for the dulling effect they can offer someone, whether in physical or spiritual pain. Adderall on the other hand is widely recognized to improve a person’s focus and seemingly require less sleep due to its stimulant nature.
Someone–we’ll name him John for this purpose–might pass one to a friend, Jackie, ensuring it’s safe and prescribed and really helps. Jane trusts John, sees his high grades on assignments and figures, “why not?”
The next day, Jane goes to school as normal, heads into her restaurant job for five hours, and later finds herself home, sitting at her desk ready to start on homework, which includes a paper due in the morning. She pauses, reaches into her pocket for the pill John gave her, and tosses it back with a swig of Coke.
The next day, Jackie and John came through the classroom doors at the same time. “Got it?” John asked. Jackie waved her paper in answer with a big thumbs up. A few days passed and Jackie texted John asking if he had an extra pill he could give to her. He quickly texted back that his prescription was low and he had to go to the doctor to get a refill but didn’t have an appointment for a few weeks and should hold on to what he had left. He signed off wishing her luck on the upcoming test.
Jackie felt frustrated. She wouldn’t normally need help focusing or staying awake but was feeling pressure between school and work. She had told her doctor that at her last annual appointment. He suggested if it became too much, Jackie could reduce her credit hours and consider making a class up in the summer, which would lessen her load daily. There’s no way he would just give her a prescription.
But she had a way around that:her sister’s prescription. Jackie made sure to stop by her home that weekend for a visit with her parents and younger sister. She also made sure to leave after pouring half of her sister’s prescription in a sandwich baggie to use later.
The example above is one of many typical ways in which a person not prescribed medication might start taking it. A trusted friend offers, it’s not an illegal drug, and it helped. The natural path that often results is they then become desperate for more and begin stealing from family or friends or buying from strangers.
How Common Is Alcohol and Adderall Usage?
Several studies have corroborated each other indicating prescription-holders have been asked for medication from others, as well as people admitting they have used someone else’s medication. While various studies have tracked use by age, the following are just two examples. A sample of middle- to high-school-aged students in the Midwest showed 23% of students with a prescription to treat ADHD reported they had been approached to sell, trade, or give their medication to someone.
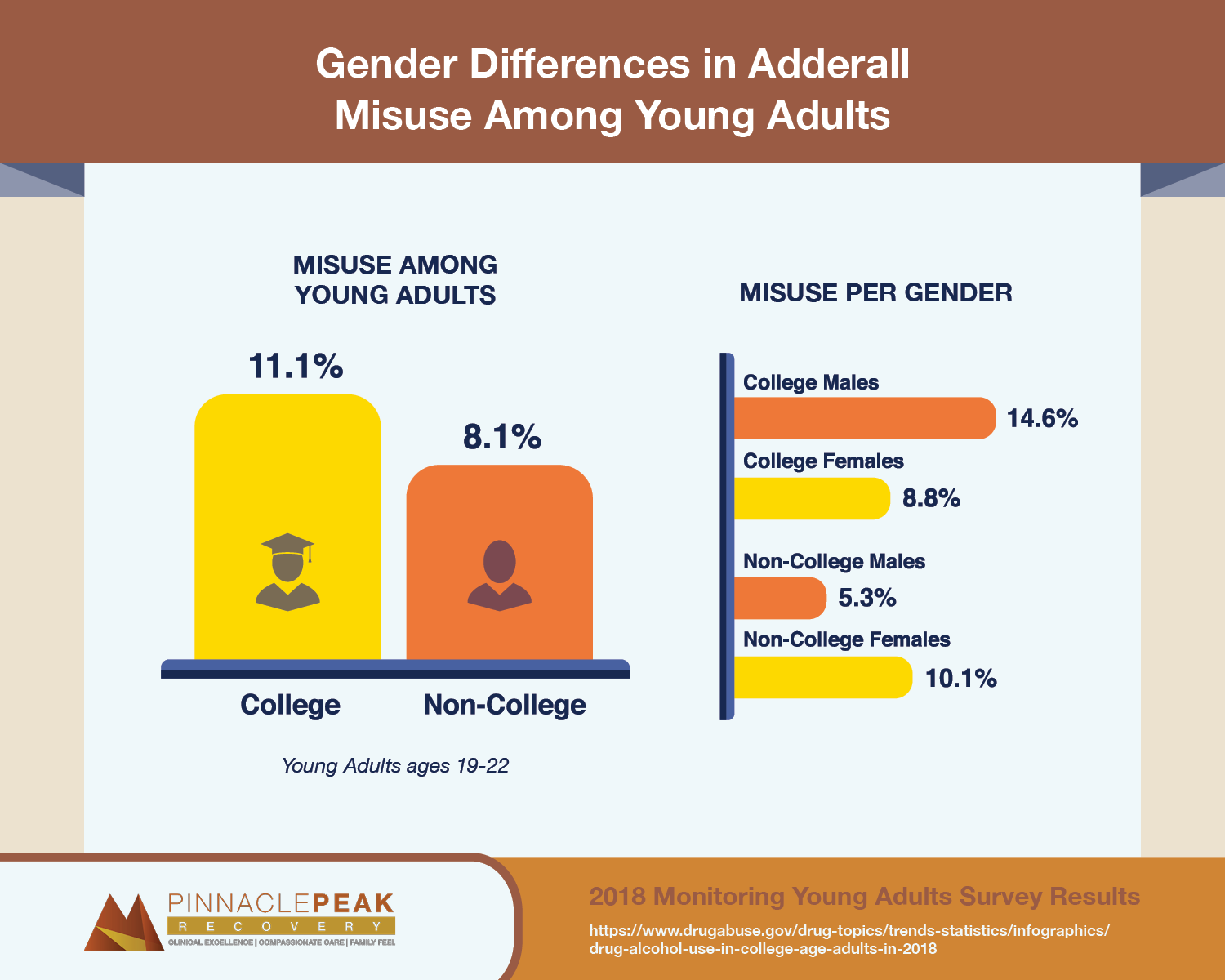
A 2018 survey by the National Institute for Drug Abuse found that of adults ages 19-22, 11% of college students and 8% of non-college adults admitted to misusing Adderall in the past year. Interestingly, gender showed 15% male vs 9% female misusing in college but a reversal in non-college adults with 5% male and 10% female misusing.
Why is it addictive?
Adderall is an amphetamine, categorized by the United States Drug Enforcement Agency (DEA) as a Schedule II controlled substance, meaning that the risk of addiction or potential for abuse is high.
Knowing this, the medical field is careful in diagnosing patients that may benefit from medication to treat ADHD or if there are other options to help them manage their symptoms. The study cited earlier showed more than seven percent of adults ages 18 to 49 years abused ADHD medications.
When we discuss the dangers of mixing Adderall with alcohol, consider this very sobering statistic: alcohol is the substance most commonly used in combination with ADHD drugs.
Signs of Addiction to Adderall
Like many medications, Adderall side effects are similar to those already identified, such as heart palpitations, dizziness, or lack of sleep. The presence of these health conditions might indicate the presence of substance misuse. Behavioral changes such as stealing or lying to get medication, problems with school and work performance, and family relationships are other signs there could be a problem.
Even if addiction is not present, misusing a prescription medication and having no medical supervision can have serious consequences. Adding alcohol to a stimulant adds more severity to the situation.
How Adderall and Alcohol Interact
While some use Adderall for legitimate medical reasons, many individuals recreationally use this prescription medication. Doing so can be very dangerous, but mixing Adderall with alcohol brings even greater risks.
For people seen in emergency rooms for Adderall interactions, 20% had also consumed alcohol. By learning how Adderall and alcohol interact, you can see just how dangerous this combination can be.Increased Chance of Alcohol Poisoning
Those who use Adderall may not feel the effects of alcohol as quickly. The internal cues they rely on to determine that they’ve had too much to drink might not appear as they usually do. For many people, particularly young people, this can lead to drinking too much. If you or someone you know want to break free from alcohol addiction, Pinnacle Peak Recovery can get you on the path to recovery in our alcoholism treatment program.
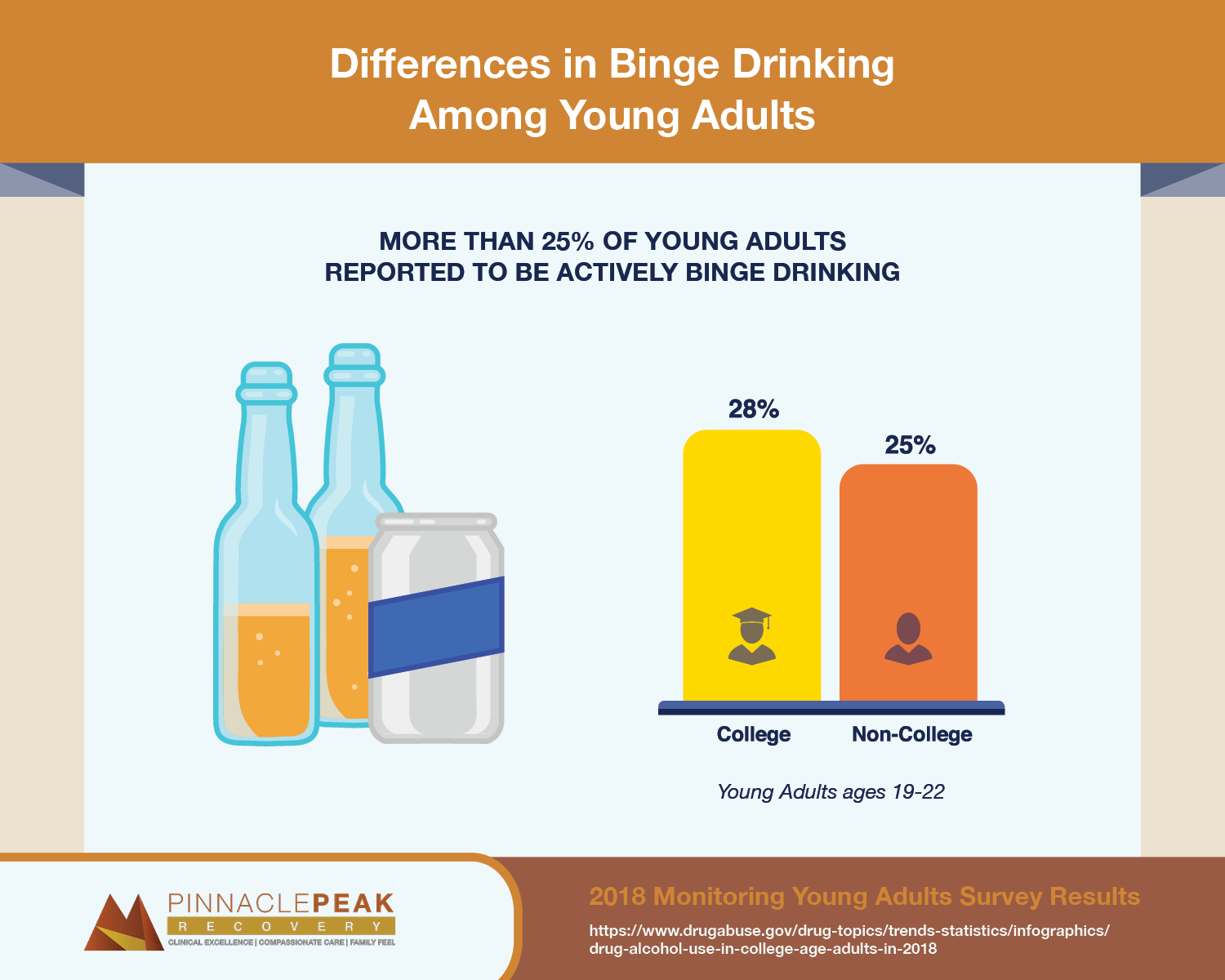
On a positive note, binge drinking (defined as five or more drinks in a sitting within the past two weeks) fell below 30% for the first time in 2018. It was reported by 28% of college students and 25% of non-college adults between the ages of 19-22.4
In some cases, drinking while on Adderall can lead to alcohol poisoning, passing out, or risking serious bodily injury.
Increased Rates of Paranoia, Anxiety, and Depression
Experts link drinking alcohol in excess to increased rates of mental health problems like paranoia, depression, and anxiety. Adding Adderall to the mix only increases the likelihood of these mental health disorders. These conditions can arise while a person is drinking, but they may also crop up the next day. Combining Adderall hangover with these conditions only worsens their severity and makes them harder to overcome.
Stimulants and Depressants Don’t Cancel Each Other Out
There’s a common misconception that Adderall abuse and alcohol can somehow cancel each other out. While it’s true that Adderall is a stimulant and alcohol is a depressant, they still both retain their effects.
Your body will still take on the stress and impact of both substances. Rather than canceling each other out, mixing Adderall with alcohol can worsen the effects of both.
The Combination Can Lead to Behavioral Issues & Side Effects
Drinking alcohol lowers inhibitions, which can often lead to risky or unsafe behavior. It can also lead to aggression. Adding Adderall to the mix heightens this, leading to riskier, more unsafe, and more aggressive behavior. Things like fights, car accidents and criminal activity might be more likely when you mix substances such as alcohol and Adderall.
Adderall and Alcohol Can Cause Heart Problems
As we’ve pointed out, Adderall causes heart problems for some individuals. It can also increase your heart rate and blood pressure or cause an irregular heartbeat. When individuals drink alcohol at the same time, they’re at a greater risk for all of these cardiac conditions. At high doses, prescription stimulants can lead to dangerously high body temperature, an irregular heartbeat, heart failure, and seizures.
While no one should mix alcohol and Adderall, those who are particularly at risk for heart conditions should take care to never, ever do so.
Alcohol Addiction Co-occurring May Be Considered
If a person is misusing Adderall and happens to have a few drinks socially, this has already been stated to be dangerous for potential heart issues and other side effects. If alcohol is also being misused with high consumption levels, this is called a co-occurring disorder. A professional can help determine if that diagnosis is accurate.
Treatment for Adderall & Alcohol Abuse
Individuals who misuse both alcohol and Adderall may benefit from dual diagnosis treatment. Treatment for this type of addiction often requires a variety of therapies that address withdrawal symptoms, root causes, and thought patterns leading to addictive behaviors.
There is no single addiction treatment that helps everyone. Getting help for addiction involves a complete overhaul in the way a person thinks, feels, and interacts with the struggles of daily life.
Treatment at Pinnacle Peak Recovery takes a holistic approach in treating the person as a whole: mind, body, and spirit. You will gain a full understanding of the underlying causes that directed you to find substance use a viable option. In turn, you will develop new skills to cope with life’s journey without substances. For many people, this involves a variety of therapies.
As counselors get to know you, they find out what therapies are best for your recovery. For example, an exercise or yoga program may aid your desire to improve physical health and provide stress release as a therapeutic alternative to medication.
At Pinnacle Peak we emphasize clinical excellence, compassionate care, and a family feel. We also strive to maintain connections after discharge, because the longer a client is connected to care the better their chances for recovery. Call Pinnacle Peak to see how our recovery program can begin your path to healing. Call 866-377-4761.
Adderall and Alcohol FAQs:
How Long After Taking Adderall Can I Drink Alcohol?
Adderall is generally prescribed in a low-dose, short-acting stimulant level lasting approximately four hours, or in a higher-dose, longer-acting level lasting longer into the day. There are no specific guidelines on a safe level of alcohol use other than abstaining. Some doctors recommend a patient may have no more than a single drink and only once the effects of medication are fully subsided.
Can You Drink Alcohol While Taking ADHD Medication?
Alcohol can cause the long-acting stimulant medication to be released too quickly leading to dangerous side effects and overdose, even taken in the prescribed dosage. There are no specific guidelines on a safe level of alcohol use other than abstaining.
Why Is it Bad to Mix Alcohol?
Adding alcohol to ADHD medication complicates the already serious side effects that are possible with the medication and can cause increased heart rate, blood pressure, mood disorders, and drowsiness.
Alcohol can also trigger the prescription drug to release earlier than planned under the time-release, causing toxicity and overdose, even if the prescribed level was taken.
Do You Burn More Calories on Adderall?
One possible side effect with Adderall is decreased appetite, which can lead to burning more calories as your body looks for nutrients. This period is often short-lived and a strong appetite usually occurs after the medication begins to wear off.
A proper nutrition plan to balance this appetite swing can be helpful, such as a protein smoothie early in the day, with health snacks added throughout the afternoon, to prevent an extreme desire to consume a high amount of calories at once later in the day.

